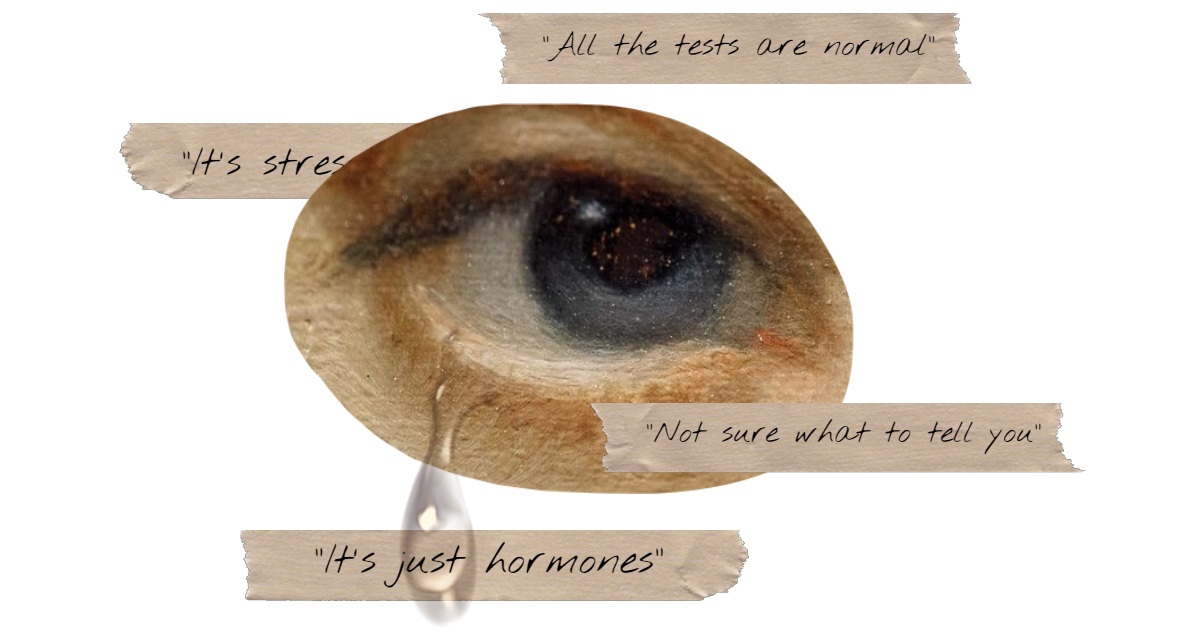
As a society, we’ve made significant progress in recent years towards greater equality and understanding. However, when it comes to women’s health, there’s still a long way to go. In this article, I’ll be exploring the devastating cycle of misdiagnosis that many women face in Western medicine, and the ways in which we can work towards breaking this cycle.
Disclaimer
Before we dive in, I want to acknowledge that health issues are complex and multifaceted, and there are many potential causes for any given symptom. This article is not meant to be a comprehensive guide to all possible health issues, but rather a commentary on the systemic problems within Western medicine that can lead to misdiagnosis. It’s crucial for individuals to take an active role in their healthcare by researching their symptoms, asking questions, and seeking a doctor who truly listens and believes their concerns.
The Statistics
The statistics are staggering. Each year, approximately 1 in 20 people in the United States are misdiagnosed. This statistic underscores the gravity of the situation and the widespread nature of diagnostic errors. According to the National Institutes of Health (NIH), women are 30% more likely to experience misdiagnosis than men. Women are also more likely to be diagnosed with mental health issues unrelated to the root cause of them.
Misdiagnosis can occur across various medical conditions, from common ailments to more serious diseases, leading to inappropriate treatments and unnecessary distress for patients. These statistics emphasize the importance of addressing diagnostic accuracy to improve patient outcomes and trust in healthcare.
Causes and Effects
The causes of misdiagnosis are multifaceted, often stemming from systemic issues within the healthcare system. One primary cause is the failure to order follow-up tests, which can lead to incomplete understanding of a patient’s condition. Additionally, misinterpretation of scans and diagnostic images can result in incorrect diagnoses.
One of the reasons for this cycle of misdiagnosis that disproportionately effect women is the lack of understanding about women’s health within the medical community. Women’s bodies are often viewed as “mysterious” or “complex,” which can lead to a lack of knowledge and confidence among healthcare providers. This can result in a failure to diagnose or treat conditions that are specific to women’s health.

The effects of misdiagnosis are far-reaching and can be devastating. Patients may incur the cost of useless treatments and additional appointments, leading to financial strain. Unnecessary treatments not only waste resources but can also take a physical toll on patients, causing side effects and complications. In some cases, a misdiagnosis can delay the correct treatment, worsening symptoms and potentially leading to severe consequences, including death. These issues highlight the critical need for improved diagnostic procedures and greater awareness among healthcare providers to minimize the risk of misdiagnosis.
The Unseen Bias: Lack of Medical Research on Women
The lack of understanding about women’s health is not only a result of the medical community’s lack of knowledge and confidence, but also due to the historical lack of medical research on women. Women’s bodies have been overlooked and underrepresented in medical research, leading to a significant disparity in the way conditions are diagnosed and treated.
For example, autism has been primarily researched in men, with many misconceptions about how autism presents itself in women. As a result, many women with autism go undiagnosed or are misdiagnosed with mental health disorders like bipolar disorder. This is just one example of the widespread issue of women being overlooked in medical research.
The invisibility of women’s health issues is not limited to autism. Many conditions, such as endometriosis, polycystic ovary syndrome (PCOS), and premature ovarian failure (POF), are still poorly understood and underdiagnosed. Women’s unique experiences and biology are often overlooked or ignored, leading to inadequate treatment and a lack of effective care.
The consequences of this lack of research are far-reaching. Women are often subjected to unnecessary procedures, misdiagnosed with conditions that were falsely diagnosed, and may not receive proper treatment for their conditions. This can lead to delayed diagnoses, incorrect treatment, and even further complications.

Breaking the cycle of misdiagnosis requires a fundamental shift in the way we approach medical research and treatment. It requires recognizing the value and importance of women’s health, and prioritizing research that addresses the specific needs and experiences of women. By acknowledging the historical lack of research on women and addressing these disparities, we can work towards creating a more equitable and effective healthcare system for all individuals.
Breaking the Cycle
So, what can be done to break this cycle of misdiagnosis? First and foremost, it’s essential for individuals to take an active role in their healthcare by researching their symptoms, asking questions, and seeking a doctor who truly listens and believes their concerns. This may involve seeking out a specialist or a doctor who has experience treating women’s health issues.
Researching commonly misdiagnosed issues often overlooked by Western medicine can also be an excellent starting point. While not exhaustive, it provides a solid foundation. To learn more about some of the most commonly misdiagnosed issues, check out our article on health issues that are often overlooked or misdiagnosed. This resource is not for self-diagnosis but can help you know what to ask your doctor to test for.
Conclusion
In conclusion, the cycle of misdiagnosis is a serious issue that affects many women worldwide. While there are many potential causes for any given symptom, it’s essential for individuals to take an active role in their healthcare by researching their symptoms, asking questions, and seeking out a doctor who truly listens and believes their concerns. By prioritizing patient-centered care and comprehensive training on women’s health issues, we can work towards breaking this cycle and improving health outcomes for all women.
What are your thoughts on this issue? Have you experienced misdiagnosis or struggled to get an accurate diagnosis? Share your stories and comments below!
Sources
American Medical Association (AMA). (2020). Gender Bias in Medicine.
CBS News. (n.d.). 12 Million Americans Misdiagnosed Each Year, Study Says. https://www.cbsnews.com/news/12-million-americans-misdiagnosed-each-year-study-says/
CBS News. (n.d.). Because the Doctor Isn’t Always Right. https://www.cbsnews.com/news/because-the-doctor-isnt-always-right/
Harvard Medical School. (2021). The Importance of Gender-Specific Medicine.
National Institutes of Health (NIH). (n.d.). Women’s Health Research and Clinical Studies.
The Lancet. (2019). Gender Disparities in Medical Research.
UPI. (2017, April 4). Study Finds More Than 20 Percent of Patients Are Misdiagnosed. https://www.upi.com/Health_News/2017/04/04/Study-finds-more-than-20-percent-of-patients-are-misdiagnosed/7911491312817/
World Health Organization (WHO). (2018). Gender and Health.